Ilioingual Neuralgia
Ilioingual Neuralgia
Clinical Syndrome
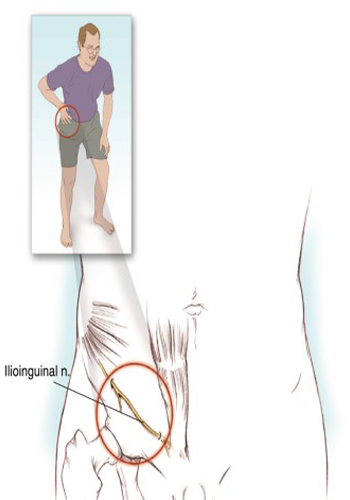
Ilioinguinal neuralgia is the most common cause of lower abdominal and pelvic pain in clinical life. Ilioinguinal neuralgia is caused by compression of the ilioinguinal nerve, and the most common causes of compression are blunt trauma is an inguinal herniophagy and traumatic pelvic surgery. Sometimes it can also be seen as spontaneous. Ilioinguinal neuralgia is characterized by paresthesia, burning sensation, and sometimes numbness in the lower abdomen, scrotum/ labia, and in the inner thigh area it is a pain that spreads correctly and does not go below the knee. The pain of ilioinguinal neuralgia can be exacerbated due to stretching of the nerve with the extension of the lumbar spine, which is why patients are inclined forward (Novice skier position). If left untreated, progressive motor loss november cause bulging of the anterior abdominal muscles. This finding can be confused with inguinal hernia. On physical examination, sensory loss can be observed in the inner thigh, scrotum and labia. There may be a weakening of the anterior abdominal wall. The Tinel sign appears where the ilioinguinal nerve pierces the transverse abdominal november.
Treatment
The treatment of ilioinguinal neuralgia can be provided with analgesics, nonsteroidal anti-inflammatory drugs and COX-2 inhibitors. Repetitive activities can aggravate the pain. Pharmacological treatment is usually not very effective however, an ilioinguinal nerve block performed using local anesthetics and steroids is necessary. The ilioinguinal nerve block is performed in the supine position. A pillow is placed under the patient’s knee; the knee can increase the patient’s pain. Palpation is performed on the anterior superior iliac and antiseptic solution is poured into the medial 6 cm and the inferior 6 cm. a 25-gauge needle with a diameter of 4-5 cm is directed to the symphysis pubis at an oblique angle. 5-7 1% lidocaine containing 40 mg methylprednisole is injected into the fascia of the external november. Aiming the needle too deeply risks penetrating into the peritoneal cavity and perforating the abdominal viscera. Post-injection ecchymosis and to reduce the formation of hematomas, pressure should be applied to the injection site. If the anatomical signs are not obvious, fluoroscopy and USG can be accompanied. In patients without a response to ilioninguinal block, the level of T12-L1 is epidural steroid injection may be considered.
