Chronic Pancreatitis
Chronic Pancreatitis
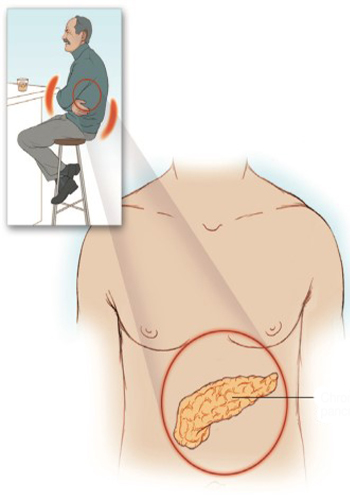
Chronic pancreatitis can occur as recurrent acute attacks. In addition to chronic pancreatic dysfunction, there may be inflammation of the pancreas or a more constant problem. The exocrine function of the pancreas is disrupted, malabsorption develops with steatorrhea (fatty defecation) and azotorrhea (nitrogenous defecation due to protein malabsorption). In the United States, chronic pancreatitis is most often caused by alcohol consumption, followed by cystic fibrosis and it is followed by a malignant pancreas. Hereditary causes such as tumors, Alpha1 antitrypsin deficiency are also common. The most common cause of chronic pancreatitis in developing countries is a lack of calories caused by severe protein deficiency it is nutrition. Chronic pancreatitis can also be caused by acute pancreatitis. Abdominal pain is a common feature of chronic pancreatitis and mimics the pain of acute pancreatitis; it ranges from mild to severe and is constant, decadent it is characterized by epigastric pain radiating to the sides and chest. The consumption of alcohol and fatty foods makes the pain worse. Nausea, vomiting and loss of appetite are also common features. Clinical picture of chronic pancreatitis symptoms are usually subject to periods of exacerbation and remission. The initial management of chronic pancreatitis focuses on relieving pain and treating malabsorption. As with acute pancreatitis, the patient is given no the pancreas is allowed to rest without giving anything. It is necessary to reduce serum gastrin secretion and, if there is an ileus, initiate nasogastric aspiration. Short-acting opioid analgesics, for example hydrocodone if prudent measures work it is a reasonable next step. If you have ileus, a parenteral opioid such as meperidine is a good alternative. The patient should be closely monitored, as opioid analgesics have the potential to suppress the cough reflex and respiration. The use of opioid analgesics should be carefully monitored, since it should be borne in mind that they have a high potential for abuse and addiction. If symptoms persist, local anesthesia with celiac plexus block under CT guidance and the steroid is indicated and can reduce the mortality and morbidity associated with this disease. If the benefit from this technique is short-term, a block of the celiac plexus with alcohol or phenol under the guidance of neurolytic CT is reasonably the next step. Alternatively, continuous thoracic epidural block with a local anesthetic, opioid, or both can provide adequate pain control and allow the patient to avoid associated respiratory depression. Hypovolemia, crystalloid and it should be treated aggressively with colloid infusions. In cases of prolonged chronic pancreatitis, parenteral nutrition is indicated to prevent malnutrition. If there is surgical drainage and severe necrotizing condition necrotic tissue may need to be removed.
